


Findings
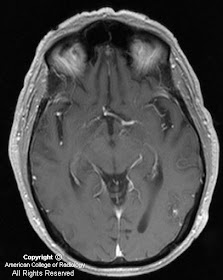
MR findings include serpiginous high and low signal (depending on flow rates) within feeding and draining vessels (Figure 1 andFigure 3). High T2 signal can be seen in the adjacent brain parenchyma secondary to gliosis, edema, or ischemia, as is seen in this case (Figure 3).
MRA reveals AVM with feeding artery branching from the left PCA. Nidus and tangled vessels are visualized (Figure 4).
Diagnosis: Arteriovenous malformation
Cerebrovascular malformations are divided into 4 major categories including arteriovenous malformation, venous angioma, capillary telangiectasia, and cavernous angioma. AVMs can be visualized with angiography, computed tomography, or magnetic resonance imaging. AVMs are the most common symptomatic vascular malformation and occur in about 0.1% of the general population. The clinical presentation is variable, including headache, seizure, and focal neurological deficits. They are occasionally discovered as an incidental finding.
AVMs are a direct communication between arterial and venous circulations and consist of a nidus of tangled dilated vessels. There are 3 subtypes that depend on the blood supply: these are pial, dural, and mixed pial-dural types. Aneurysm is associated with the feeding arteries in approximately 10% of cases. Arteriovenous shunting is usually rapid so that most vessels appear as flow voids. An AVM replaces normal brain tissue without causing mass effect, unless complicated by hemorrhage and edema. Adjacent parenchymal atrophy is common secondary to vascular steal and ischemia.
3-D TOF MRA can be diagnostically useful in demonstrating feeding arteries, the nidus, and draining veins. Occasional pitfalls in MRA evaluation include signal void in tortuous vessels, nonvisualization of draining veins resulting from spin saturation, and difficulty with differentiation of blood flow from blood clot. Conventional angiography may be necessary for treatment planning.
Nessun commento:
Posta un commento