



Findings
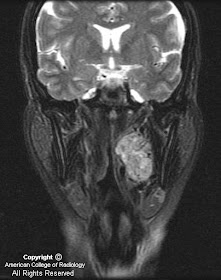
Figure 1 demonstrates a large, intensely-enhancing, heterogeneous left-sided carotid space mass displacing the internal carotid artery (ICA) medially, the external carotid artery (ECA) and its branches antero-medially, and the internal jugular vein (IJV) postero-laterally.
Figure 2 demonstrates anterior displacement of the parapharyngeal fat by the glomus vagale tumor.
Figure 3 demonstrates anterior displacement of the ICA by the left-sided fusiform-shaped glomus vagale tumor.
Figure 4 demonstrates antero-medial displacement of the ICA and posterior displacement of the IJV by the glomus vagale.
Figure 5 with arrows pointing to multiple flow voids within the left carotid space mass.
Diagnosis: Glomus vagale tumor
Paragangliomas account for only 0.6% of all neoplasms of the head and neck. They arise from the paraganlgia or glomus cells, which are part of the extra-adrenal neuroendocrine system, and are named for the paraganglia from which they arise. The four most common sites for paragangliomas of the head and neck are the carotid body (carotid body tumor), the jugular foramen (glomus jugulare), along the path of the vagus nerve (glomus vagale) and in the middle ear (glomus tympanicum). Paragangliomas are characteristically vascular, intensely enhancing lesions that demonstrate low T1 and high T2 signal with multiple flow voids. The "salt-and-pepper" appearance has been named for the T2 appearance, as the high T2 signal of the tumor is the "salt" and the multiple flow voids the "pepper".
Paragangliomas can be distinguished from each other primarily based on their location. The carotid body tumor typically splays the common carotid bifurcation, while the glomus vagale displaces both the ECA and ICA antero-medially away from the IJV. Glomus jugulare tumors characteristically expand and erode the jugular foramen causing the characteristic "moth-eaten" appearance. The glomus tympanicum is a small discrete mass arising from the cochlear promontory in the middle ear.
The current primary treatment modality is surgery with possible pre-operative embolization; radiation is reserved for non-resectable and recurrent cases and those invading the ICA. Paragangliomas have a high (40%-50%) rate of local recurrence, can be locally aggressive with intra-cranial extension (20%), and can behave in a malignant manner (2%-13% metastasize to lung, bones and lymph nodes). Familial paragangliomas (7%-9% of cases) are more commonly multiple (1/3) than sporadic cases (5%), and occur at a younger age. The primary differential diagnosis for a carotid space mass is: nerve sheath tumors, nodal metastasis (renal and thyroid cancer), abscess, and venous thrombosis.
Nessun commento:
Posta un commento