Findings
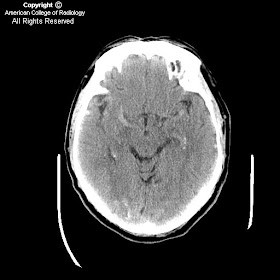
Within the medial subcortical portion of the anterior right temporal lobe, there is a 1.5 x 1.6 x 1.3 cm intraaxial lesion that demonstrates increased signal intensity on T2 and FLAIR images (Figure 2, 3, 5 and 6) and relatively low-signal intensity on T1-weighted images (Figure 1). The lesion has well-circumscribed and slightly-lobulated margins. No significant perilesional edema.
Postcontrast images do not reveal any appreciable enhancement (Figure 4 and 7).
This lesion appears to be located inferior and mostly anterior to the right amygdala, and expands the right parahippocampal gyrus medially and the right fusiform gyrus inferiorly.
Diagnosis: Ganglioglioma
Ganglioglioma is a well-differentiated, slowly growing neuroepithelial tumor composed of neoplastic neuronal and glial elements. Majority of gangliogliomas (85%) are low grade (WHO I). It occurs most commonly in children and young adults. Patients usually have a long-standing history of seizures and headaches.
Gangliogliomas are most commonly located in the superficial cerebral hemispheres, especially the temporal lobes. These tumors are usually firm, well-circumscribed masses and may expand the involved cortex. On CT, these have an appearance of low-density or cystic masses. Focal enhancement is seen in 50% of the cases and calcification in approximately 35%. MRI demonstrates these hemispheric lesions in a cortical location, being hyperintense on T2- and hypointense on T1-weighted images. Gadolinium enhancement is variable, often focal or nodular. PET typically shows decreased activity, indicating tumor hypometabolism. In children under 10 years, gangliogliomas can be larger and more cystic.
These tumors have an excellent prognosis with complete surgical excision. The majority (80%) of the patients are seizure-free after surgery. Malignant transformation of ganglioglioma is unusual.