



Findings
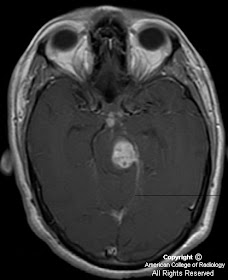
Figure 3, Figure 4, and Figure 5: Post contrast MR images show multiple coalescent ring-enhancing lesions in the left side of the midbrain and pons and in the interpeduncular and suprasellar cisterns.
Figure 1 and Figure 2: These lesions are markedly hypointense on T2-weighted images with surrounding perilesional edema.
Diagnosis: CNS tuberculosis
Tuberculous meningitis is the most common manifestation of CNS tuberculosis across all age groups.
The combination of brain parenchymal lesions and meningeal enhancement is highly suggestive of tuberculosis.
Central areas of hypointensity on T2 WI should suggest tuberculosis or fungal disease.
CNS involvement is seen in 5 % of patients with tuberculosis (TB) but prevalence increases in immunocomprised patients, being seen in up to 15% of cases of AIDS- related TB. Approximately 30 % of TB patients are HIV positive.
The disease is found primarily in children and young adults. A history of previous extracranial TB is elicited in 60%, but only 30% have concomitant manifestations of TB outside the CNS at presentation.
CNS tuberculosis usually results from hematogenous spread, often from a pulmonary source. However, it may result from direct rupture or extension of a subependymal or subpial focus (Rich focus) and may be located in the meninges, brain, or spinal cord.
CNS tuberculosis can manifest in a variety of forms, including:
- tuberculous meningitis
- tuberculomas
- tuberculous abscesses
- osteomyelitis of the skull or spine, often with associated epidural abscess
Tuberculous meningitis is the most common manifestation of CNS tuberculosis across all age groups. The typical radiographic finding is abnormal meningeal enhancement, usually most pronounced in the basal cisterns. This is best seen at gadolinium-enhanced MR imaging. Appearances usually resolve relatively quickly with adequate treatment; however, radiographic resolution is delayed if there are thickened exudates. The common complications of tuberculous meningitis are communicating hydrocephalus, ischemic infarcts or cranial nerve involvement, most commonly affecting the second, third, fourth, and seventh cranial nerves.
The acid-fast bacilli disseminate hematogeneously and lodge at the gray- white matter junction and form tuberculous granulomas. Tuberculous abscess formation with central liquefaction is rare and reflects a poor host immune response.
There are 4 stages in the evolution of tuberculomas:
- 1. Cerebritis stage: non specific edema, ill-defined enhancement
- 2. Solid, granulomatous stage: enhancing nodules with surrounding edema
- 3. Central caseation stage: central hypointensity on T2- peripheral enhancement
- 4. Involution stage- multiple calcified lesions
CNS tuberculosis has a mortality rate as high as 30 %; in HIV positive patients, it is up to 80 %. Serial imaging is useful to assess response to therapy.
Nessun commento:
Posta un commento