Findings
Figure 1: An axial CT image in bone windows demonstrates enlargement of the left labyrinthine, geniculate ganglion, and anterior tympanic segments of the facial nerve by a soft tissue mass.
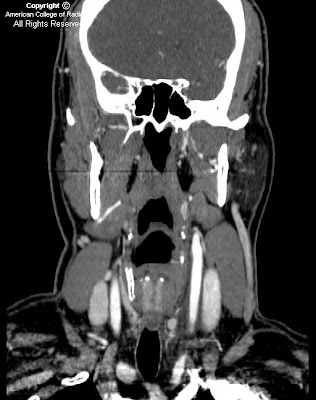
Figure 2: A coronal CT image in bone windows also shows bony expansion in the course of the left facial nerve.
Figure 3: A coronal CT image in soft tissue windows shows that there is an ovoid soft tissue mass within the geniculate fossa.
Figure 4 (T1 axial), Figure 5 (T1 axial postgadolinium) and Figure 6 (T1 coronal postgadolinium) thin slice MR images through the internal auditory canals demonstrate a tubular soft tissue mass in the geniculate fossa. Following the administration of intravenous gadolinium, this mass demonstrates avid homogenous enhancement (Figure 5).
Diagnosis: Facial nerve schwannoma
Facial nerve schwannomas (also called facial nerve neuromas) are rare benign tumors of the Schwann cells of the seventh cranial nerve. They may arise along any portion of the facial nerve, including within the internal auditory canal, the labyrinthine portion, the tympanic portion, the mastoid portion, or within the parotid gland. However, the most common location for a facial nerve schwannoma is the geniculate ganglion. Patients present most frequently with hearing loss (70%) and with slowly progressive facial nerve paralysis (50%). These lesions are slow growing, but eventually most will enlarge and cause hearing loss. The treatment may be conservative if the schwannoma is asymptomatic; these lesions may be followed until symptoms develop. Surgical treatment is also an option, with the aim being preservation of facial nerve function if possible, and facial nerve grafting if necessary. The mean patient age at presentation is 35 years. If multiple schwannomas are present, the diagnosis of neurofibromatosis type II may be considered.
Imaging of facial nerve schwannomas includes both MRI and CT. On noncontrast temporal bone CT, the findings include a tubular soft tissue mass along the course of the facial nerve with enlargement of the facial nerve canal. The bony margins are usually smooth and benign-appearing. On MRI, these lesions have intermediate to low signal intensity on T1-weighted imaging and high signal intensity on T2-weighted imaging. Following the administration of intravenous gadolinium, facial nerve schwannomas enhance homogenously. The differential diagnosis includes normal intratemporal facial nerve enhancement, Bell's palsy, facial nerve hemangioma, and facial nerve perineural parotid malignancy. Based on clinical presentation, facial nerve schwannoma can be distinguished from Bell's palsy and a hemangioma by a more gradual onset of facial nerve paralysis vs an acute onset in these other entities. Normal facial nerve enhancement is asymptomatic, and facial nerve perineural parotid malignancy is associated with a known or recurrent parotid gland malignancy. Depending on the location, facial nerve schwannomas may be indistinguishable from vestibular schwannomas in the internal auditory canal or glomus tumors within the tympanic cavity.