Findings
FindingsCT shows a basilar artery aneurysm at the level of the pons. Subtle calcification is present within the aneurysm wall (Figure 1 and Figure 2).
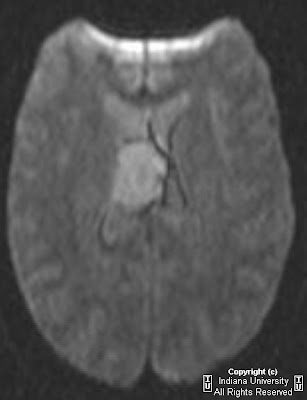
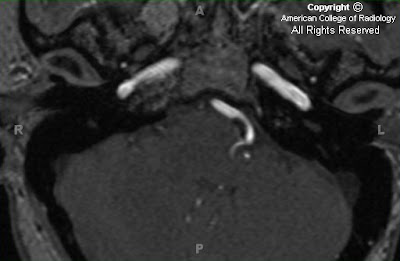
Axial GRE (Figure 5), T1 sagittal (Figure 3), T1 post gadolinium axial (Figure 6), and T2 axial (Figure 4) demonstrate a fusiform aneurysm of the mid to distal basilar artery that does not involve the basilar tip. An area of slightly increased signal intensity within the aneurysm suggests thrombus formation (blue arrow in Figure 4 and Figure 6). No subarachnoid space or fourth ventricle hemorrhage is present.
Diagnosis: Fusiform basilar artery aneurysmBasilar artery aneurysms comprise approximately 10% of all intracranial aneurysms. Fusiform aneurysms comprise only 1% of vertebrobasilar aneurysms. The fusiform aneurysm is a long segment of irregular fusiform or ovoid arterial dilatation. It is more common in the vertebrobasilar circulation than in the carotid circulation. In older adults, atherosclerosis is the most common cause of fusiform aneurysms in the basilar artery. Nonatherosclerotic fusiform aneurysms usually occur in younger patients with underlying vasculopathy or immune disorders. Fusiform aneurysms usually progressively enlarge over time. The pathologic etiology of fusiform aneuryms is partial or total absence of the internal elastic lamina and/or media, either congenital or acquired, which reduces elastic wall tension and allows subsequent expansion of the vessel diameter over time.
The saccular aneurysm is a focal dilatation of the arterial wall. The pathogenesis of saccular aneurysms reflects a combination of congenital, acquired, and hereditary factors. Large (>5 mm) aneurysms are found in 5% of the population, characteristically distributed at the arterial bifurcations. Association with polycystic kidney disease, Ehlers-Danlos syndrome, and other connective tissue disorders implicates hereditary factors.
Most intracranial aneurysms (~90%) are saccular and arise in the carotid circulation. 30-35% of aneurysms arise from the anterior communicating artery, 30-35% from the posterior communicating artery origin, 20% from the middle cerebral artery bifurcation, 5% from the basilar artery bifurcation or tip and the remaining 1-5% arise from other posterior circulation vessels. Intracranial aneurysms are multiple in 15-20% of cases. 80-90% of nontraumatic subarachnoid hemorrhage (SAH) is due to aneurysms. The risk of bleeding is approximately 2.5% per year for lesions >6mm in diameter. Complications of SAH include hydrocephalus, rebleeding, and vasospasm.
On non-enhanced CT, the aneurysm is hyperdense, and calcification in the wall may sometimes be detected. Aneurysmal SAH may be detected in 90-95% of cases on non-contrast head CT. CTA may detect aneurysms greater than 3 mm, providing detailed evaluation of morphology such as the relationship to the parent vessel and the neck width. CTA can detect more than 95% of aneurysms identified on conventional angiography. MRI demonstrates variable signal on T1 weighted images, hypointense lumen and clot on T2 weighted images, and strong enhancement of the residual lumen on post-contrast T1 weighted images. CTA or dynamic contrast-enhanced 3D-TOF MRA are the studies of choice for evaluation as non contrast 3D-TOF images are suboptimal due to flow saturation and phase dispersion. Conventional angiography is the definitive procedure for the detection and characterization of cerebral aneurysms. Aneurysm location, size, and morphology may be evaluated in the acute or chronic setting with this modality.
Management of fusiform aneurysms is difficult due to their morphology. Occlusion of the parent arteries, “Hunterian ligation,” is advocated as the preferred method of treatment. The “Alskock Test” is usually performed to evaluate patency of the posterior communicating (PCOM) arteries by compressing the cervical carotid artery during contrast injection of the vertebral artery. A PCOM greater than 1 mm can be visualized and suggests the possibility of collateral flow after occlusion of the vertebrobasilar system. Endovascular occlusion of basilar and vertebral arteries with balloons and coils is used in nonatherosclerotic fusiform aneurysm cases with good results. There are reports of successful treatment of ruptured basilar aneurysms with stent-graft placement from the vertebrobasilar junction to the midbasilar artery.