



Findings
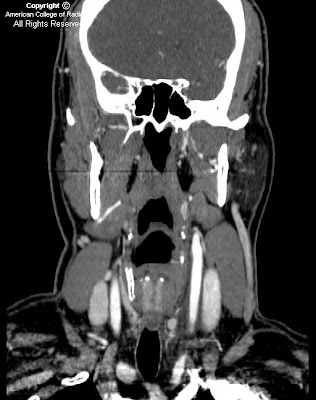
On axial source image (Figure 1) and coronal (Figure 2) reformatted CTA of the neck, there are inflammatory changes and soft tissue attenuation surrounding the left common carotid artery consistent with thickening of the carotid sheath. Compare this with the normal right carotid artery (Figure 1). The left carotid artery itself is normal, without significant narrowing or evidence for dissection.
Axial T1 precontrast (Figure 3) and postcontrast (Figure 4) images demonstrate enhancement of the carotid sheath on the left (Figure 4). On T2-weighted images, there is increased signal (Figure 5) in this region as well.
Brief differential for neck pain:
- Atherosclerosis or thrombosis
- Aneurysm, aneurismal dissection, or intraluminal hemorrhage
- Giant cell arteritis
- Fibromuscular dysplasia
- Lymphadenitis
- Submandibular gland disease
- Carotid body tumor
- Migraine-associated pain
- Idiopathic carotidynia
Diagnosis: Idiopathic carotidynia
Carotidynia is a syndrome of unilateral neck pain with tenderness to palpation over the carotid artery, first described in 1927. Neck pain can have many causes, and it is important to exclude other etiologies before a diagnosis of idiopathic carotidynia can be made. In this case, we describe the characteristics of idiopathic carotidynia, which is a benign, self-limited syndrome. There is controversy whether the entity even exists, and some have suggested that the diagnosis is not validated.
The etiology of idiopathic carotidynia is proposed to be inflammatory; the syndrome is often associated with a preceding viral illness, occurs more frequently in cold weather, and is more common in women than men. The inflammatory nature is supported by its prompt response to steroids and NSAIDS, and a postviral etiology is supported by its self-limited course. Limited pathologic confirmation exists due to the benignity of the syndrome and obvious risks of biopsy. However, there is a pathologic case report describing a biopsy taken during a CEA, which demonstrates localized inflammation not characteristic of that seen in a typical vasculitis.
Benign, idiopathic carotidynia is a diagnosis of exclusion, and although diagnosis can be made clinically, imaging is important in uncertain cases and to exclude other causes of neck pain. MR is the preferred examination. Typically, on T1-weighted images, abnormal enhancing tissue conforming to the fascial borders of the carotid sheath is seen, and increased signal in the same region is present on T2-weighted images. Computed tomography findings are similar, demonstrating homogenous soft tissue infiltration of the carotid sheath and surrounding inflammatory changes. No associated narrowing of the lumen is present.
Although benign idiopathic carotidynia is self-limited by definition, many patients are treated with a short course of NSAIDS or steroids for symptom relief. Prompt response to treatment confirms the diagnosis. In these cases, the lack of any other findings to suggest an alternative diagnosis supports the existence of carotidynia as a distinct clinical syndrome.
International Headache Society Classification Committee criteria for the diagnosis of idiopathic carotidynia:
A) At least one of the following overlying the carotid artery:
- Tenderness
- Swelling
- Increased pulsations
B) Appropriate investigations do not reveal a structural abnormality
C) Pain over the affected side of the neck; may project to the ipsilateral side of head
D) Syndrome is self-limiting, of less than two weeks duration
Nessun commento:
Posta un commento