





Findings
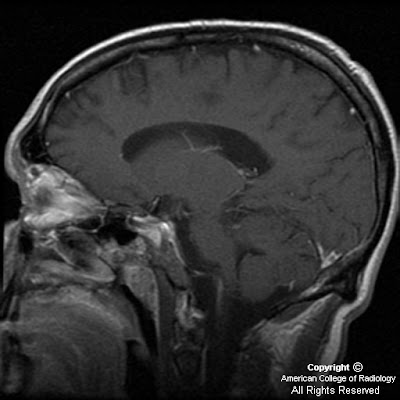
MRI shows multiple foci of hypointensity on T1 and hyperintensity on T2 and FLAIR throughout the subcortical white matter of bilateral frontal, temporal and parietal lobes. Similar lesions are seen in left pons and right cerebellar hemisphere. Figure 2 and 3, which are FLAIR images, demonstrate well the involvement of the subcortical U-fibers. There is no significant mass effect associated with these lesions. No appreciable enhancement is seen on postcontrast images (Figure 4, Figure 5, Figure 6, and Figure 7).
Diagnosis: Progressive Multifocal Leukoencephalopathy (PML)
Progressive Multifocal Leukoencephalopathy (PML) is a fulminating opportunistic infection of the brain caused by JC virus. The virus is commonly latent in the central nervous system (up to 80% of adult population is infected) but targets the oligodendrocytes in immune compromised patients. It occurs in AIDS patients with very low (less than 50-100) CD4 counts.
PML typically results in progressive neurologic decline in AIDS patients, but can be the presenting illness.
The need to diagnose and treat PML is urgent in patients with HIV as the infections are synergistic. Brain biopsy was previously required for definitive diagnosis. With positive JCV Polymerase Chain Reaction CSF results and MR findings characteristic of PML, brain biopsy can be avoided in many AIDS patients.
On CT, it presents as focal, bilateral, asymmetric, usually well-demarcated areas of low attenuation, typically in the subcortical and periventricular white matter.
MRI reveals asymmetric, multifocal areas of T1 and T2 prolongation in the periventricular and /or subcortical white matter. Involvement of subcortical U-fibers is common, giving a “scalloped” appearance to the lateral margins of the lesions. Classically, the lesions occur in the parieto-occipital white matter. However, lesions may involve any part of cerebral hemispheres as well as brainstem, cerebellum, and basal ganglia. Mass effect and enhancement are usually absent or mild, if present. Marked mass effect or robust contrast enhancement should suggest alternative diagnoses.
HIV encephalitis is the leading diagnostic possibility in the differential diagnosis of non- enhancing, non-mass-producing white matter lesions in patients with AIDS. White matter changes in HIV encephalitis are usually symmetrical and diffuse. Posterior fossa is also uncommonly involved with HIV encephalitis.
There is no specific therapy for PML, and it was previously considered to be fatal with median survival being around four months. Improved patient survival has been reported with HAART (highly active antiretroviral therapy).
Nessun commento:
Posta un commento