Findings
Figure 1, Figure 2, and Figure 3: Sagittal T2 and post contrast sagittal T1 weighted images demonstrate numerous enhancing intradural, extramedullary masses lining the roots of the cauda equina.
Figure 4, Figure 5, and Figure 6: A heterogeneously enhancing right paraspinal mass demonstrates heterogenous signal on T2 weighted images, highly suggestive of a schwannoma. There is no adjacent osseous erosion.
Diagnosis: Schwannomatosis
Schwannomatosis is a form of neurofibromatosis that has unique diagnostic criteria but can have findings that overlap with other forms of NF that can confound diagnosis.
Spectrum of neurofibromatosis:
- Neurofibromatosis Type I: Café au lait spots, skin fold freckling, Lisch nodules, cutaneous and plexiform neurofibromas, learning disabilities, and propensity for malignancy
- Neurofibromatosis Type II: Bilateral vestibular schwannomas, various other intracranial, spinal and cutaneous schwannomas, meningiomas, ependymomas. Ocular manifestations include cataract, retinal hamartoma
- Schwannomatosis: Schwannomas in multiple locations without the presence of vestibular schwannomas
Schwannomatosis, also known as neurilemmomatosis, is a condition of multiple non-vestibular schwannomas in a patient who has no other stigmata of neurofibromatosis type 2. Schwannomas are benign nerve sheath tumors that are usually solitary and occur sporadically. A definite diagnosis of schwannomatosis can be made when a patient older than 30 years has two or more nondermal schwannomas, one of which has been pathologically confirmed. There is however, a wide spectrum of overlap between schwannomatosis and NF2 such that a definitive diagnosis may be difficult to make.
Differences between schwannomatosis and NF2 include the age of presentation. Most patients with the former will present in middle age, whereas patients with NF2 present in the second to third decade of life. Patients with schwannomatosis generally do not have a corresponding family history, unlike NF2.
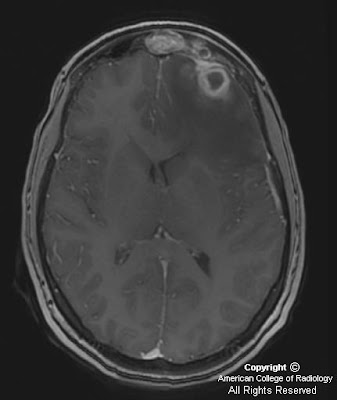
Imaging characteristics of the tumors in schwannomatosis are the same as those of sporadic schwannomas. Iso/hypointensity on T1 weighted images, hyperintensity (secondary to cystic change, and occasionally hemorrhage) on T2 weighted and STIR images and avid contrast enhancement are typical findings.
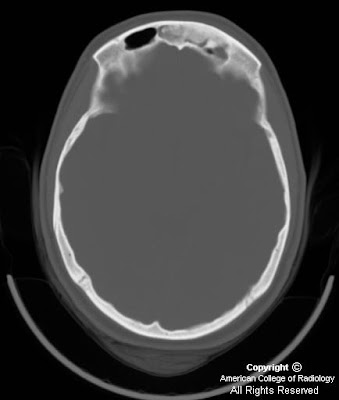
Dedicated imaging of the internal auditory canals and the brain should be pursued to help clarify the diagnosis. Follow up imaging is also indicated, especially if the diagnosis is not definitive, as malignant degeneration of an NF2 lesion would manifest as rapid increase in size of a mass.