Findings
Two sagittal T2 images (Figure 1 and Figure 2) in a trauma patient. There is an acute compression fracture of the T11 vertebral body with retropulsion of the posterior cortex. There is loss of CSF signal between the posterior vertebral cortex and the spinal cord and there is deformity of the cord at the fracture site. Increased T2 signal is seen in the cord at this level.
Axial T1 image (Figure 3) demonstrates the fracture with associated cord compression, less well seen than on the T2 images. Abnormal signal adjacent to the cord is consistent with subacute hemorrhage.
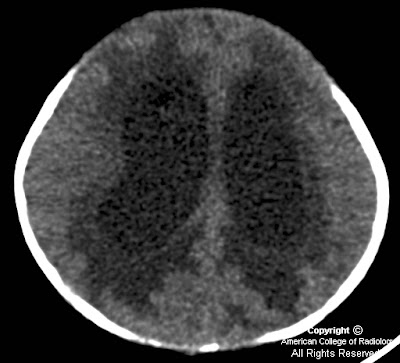
Axial T2 image (Figure 4) confirms the fracture, loss of CSF between the cord and adjacent bone (Figure 4), and the two bright foci of signal abnormality within the cord. This increased T2 signal is seen within the central gray of the cord with sparing of the white matter tracts, a common initial presentation of cord edema. Additional bony disruption is seen on the left.
Diagnosis: Post-traumatic fracture with cord compression
Acute spinal cord compression is a potentially devastating neurological emergency that requires both prompt diagnosis and intervention to prevent permanent impairment. Close cooperation between clinical services and diagnostic radiologists is essential for patient triage. This is especially true in cases where patients cannot be fully examined neurologically. Magnetic resonance imaging is the study of choice in the evaluation of these patients, as it is noninvasive, does not involve radiation, and provides for investigation of both osseous and soft tissue lesions.
Information from the neurological exam is critical for localization of the lesion and optimization of the imaging protocol. Whole spine imaging is generally undesirable, as it is more time-consuming, expensive, and difficult for patients who are often in considerable pain. It further lowers resolution on exams that are often suboptimal secondary to severe patient pain and patient movement. Spinal sensory levels on neurological examination may be up to several segments below the anatomic level of cord compression. Evaluation of motor function and reflexes is very useful for lesion localization.
Once the site of interest is more precisely identified, sagittal T1 and T2 images and axial T2 images are required for the diagnosis. Axial T1 images through the lesion may then be obtained for further characterization of the anatomy and evaluation of hemorrhage. Intravenous contrast is not necessary for the diagnosis of acute cord compression.
Spinal cord compression may be defined as the presence of a mass lesion abutting the cord with the complete loss of intervening CSF. This must be accompanied by deformation of the spinal cord, or the presence of signal changes within the cord. The findings are best visualized on T2-weighted images. If the patient is concurrently symptomatic, acute intervention is mandated with the specific type of intervention determined by the underlying disease process. In acute cord compression secondary to trauma, imaging findings may also have prognostic value separate from findings on neurological exam.