Findings
Figure 1 (26-day-old neonate). An arrow points to cysts within the brain parenchyma anterior to the right frontal horn. An even larger area of cysts is seen anterior and lateral to the left frontal horn. The cysts are consistent with a diagnosis of cystic periventricular leukomalacia. The ventricles are normal in size. There is no evidence of intraventricular hemorrhage.
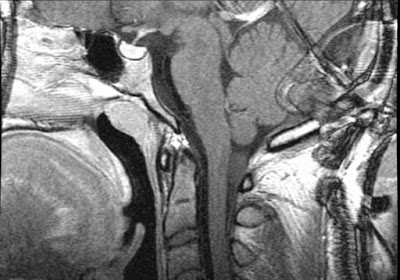
Figure 2 (4-day-old neonate). The brain appears normal. Choroid plexus is seen in each normal-sized lateral ventricle. The anterior watershed area cysts seen 22 days later (Figure 1) are not seen. Ventricles do not parallel each other, but rather extend toward each other suggesting that lines drawn through them would meet if extended anteriorly. This fact goes against the diagnosis of agenesis of the corpus callosum.
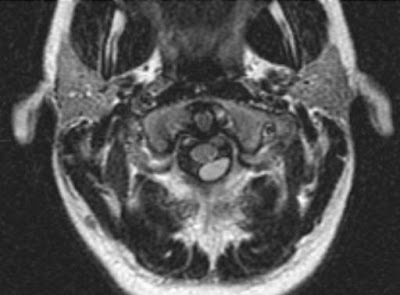
Figure 3(26-day-old neonate). Cysts are noted within the brain parenchyma in the right peritrigonal area. No ventriculomegaly is seen.
Figure 4 (4-day-old neonate). Some bright echogenicity is seen anteriorly in an area just lateral to the frontal horn of the right lateral ventricle. A larger area of bright echogenicity is seen in the right ventricle's peritrigonal region. Whether this is normal echogenicity that may be caused by the anisotropic effect as the sound beam crosses normal white matter fibers in the region at 90 degrees or this is very subtle echogenic PVL, could not be determined at the time of the US examination.
Diagnosis: Periventricular leukomalacia
Perhaps the most significant pathologic injury that can occur to the premature brain during neonatal life is periventricular leukomalacia (PVL). It is an ischemic abnormality thought responsible for the later development of spastic diplegia and intellectual deficits including learning disorders. It is a major cause of cerebral palsy in children. It is due to necrosis of cerebral white matter at arterial borders (watershed areas). Optic radiations at the ventricular trigone and cerebral white matter just lateral to the frontal horns are the most commonly affected areas noted on US. It was only first described on CT in 1978 and US in 1983. PVL has been well-documented in association with obvious perinatal problems, but has also been noted in newborns without them.
PVL may be difficult to diagnose during its acute phase when affected areas are echogenic, but may appear similar to the normal echogenic periventricular white matter seen surrounding the lateral ventricles, particularly on coronal views. Asymmetry, when comparing right to left sides may be the only hint something is amiss. The echogenic peritrigonal area seen in normal neonates is thought to be due to the anisotropic effect of the US beam passing from its entry at the anterior fontanelle to the white matter fibers in the peritrigonal area at a 90 degree angle.
Although the echogenic phase of PVL may be difficult to separate on US imaging from areas of normal brain, the diagnosis becomes quite easy within 2-3 weeks, when the cystic phase of PVL develops. The cysts are far more readily seen and are quite distinguishable from normal solid brain parenchyma, as noted in our test images. The best areas to note this on US are on either side of the brain, anterior and lateral to the frontal horns (an anterior watershed area) and posterior to the lateral ventricles in the peritrigonal area (a posterior watershed area).
These cystic areas eventually are filled in by gliosis. When this occurs, US will no longer show the abnormality. This suggests that timing is of the essence in making the diagnosis. Some pediatric radiologists recommend head US exams to be performed on at risk premature infants who are asymptomatic at least 2-3 times during their neonatal course. An exam in the first week (day 4-7) is to be performed to analyze for IVH, one at 2-3 weeks for posthemorrhagic hydrocephalus or cystic PVL, and one at 12 weeks if head growth chart readings are of concern and there is, therefore, further concern to diagnose late hydrocephalus.