Findings
Poorly defined, diffusely increased signal is noted on T2-weighted images (Figure 1) involving predominantly the right frontal and parietal lobes. This abnormal signal involves predominantly the white matter but extends to the adjacent cortex, to the insular cortex and inferiorly involves the thalamus and posterior limb of internal capsule to reach the upper mid brain.
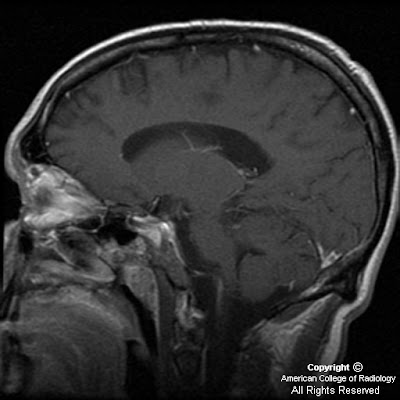
These lesions are iso- to hypo-intense on T1WI (Figure 2). For the size of the lesion, there is not much distortion of the anatomy and there is little mass effect on the ipsilateral lateral ventricle with slight shift of midline to the left.
On the post contrast images (Figures 3, 4 and 5), there are only scattered foci of enhancement in the centrum semiovale and parasagittal gray matter (Figure 3). Foci of enhancement likely represent areas of dedifferentiation.
Figure 6: MR Spectroscopy reveals slight increase in the choline peak and slight reduction of NAA peak.
Diagnosis: Gliomatosis cerebri
Gliomatosis cerebri is an uncommon primary brain tumor characterized by diffuse neoplastic proliferation of astrocytes, with relative preservation of underlying brain architecture and sparing of neurons. By definition, it is infiltrative, involving at least two lobes of the brain, frequently bilateral. Usually WHO Grade III, it is differentiated from multifocal gliomas based on continuity of cellular infiltration and lack of clear distinction from adjacent normal brain tissue.
Patients usually present between the 3rd and 5th decades of life. Clinical findings are nonspecific and characteristically mild in comparison with imaging findings. The process shows a relentless progression over time and typically presents with a slow decline in cognitive function.
The areas infiltrated by neoplastic astrocytes include (in decreasing order of frequency) the cerebral hemispheres, basal ganglia, thalami, corpus callosum, brainstem, spinal cord and cerebellum. The tumor typically crosses the midline and involves at least two, usually three lobes of the brain. Hemispheric white matter involvement is typical, but the cortex may also be involved in approximately 20% of cases.
CT may demonstrate normal findings or may show ill-defined asymmetric low density with minimal or no enhancement. MRI is more sensitive, but also often underestimates the extent of disease. The tumor appears as infiltrating hyperintense mass on T2 WI with enlargement of involved structures. Enhancement may indicate malignant progression or a focus of malignant glioma. Vascular proliferation and necrosis are typically absent.
MRS and dynamic contrast-enhanced T2*-weighted imaging help further characterize the tumor.
Stereotactic biopsy may be guided by an enhancing nodule if present, or by the area of maximum Choline/NAA increase.
The prognosis is generally poor with 50% mortality at one year. Steroid therapy may be helpful in the short term. Radiation therapy and chemotherapy are of questionable benefit.