Findings
FindingsFigure 1: Sagittal T1 FLAIR image shows subtle distortion of the anatomy at the conus and proximal cauda equina. No mass is seen.
Figure 2: Sagittal T2 weighted image shows subtle distortion of the anatomy at the cauda equina. There is a suggestion of a T2 hyperintense lesion splaying the roots of the cauda equina.
Figure 3: Axial T2 weighted image shows centrifugal displacement of the nerve roots of the cauda equina. There is T2 hyperintense material, similar in signal to CSF, centrally.
Figure 4: PA and lateral views from a contrast myelogram following introduction of 10 cc of Isovue 200M into the subarachnoid space shows six lumbar vertebral bodies and a complete myelographic block by a convex bordered mass at L2-3.
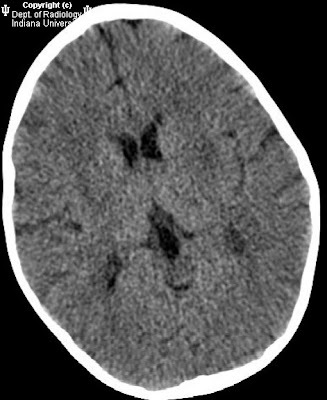
Figure 5: 20-minute delayed sagittal and coronal reformatted images from CT-myelogram shows the almost round cyst at L2 causing an incomplete block (there is a mild amount of contrast above the cyst). Note the cyst contents do not communicate with the sub-arachnoid space and hence the cyst remains low density (dark). The cyst is splaying the nerve roots of the cauda equina and posteriorly displacing the filum terminale tethering the conus medullarus posteriorly.
Diagnosis: Spinal Arachnoid CystSpinal arachnoid cysts are uncommon and may be extramedullary-intradural or epidural. They are CSF fluid sacs contained by arachnoid. Clinical presentation is variable including pain, weakness, numbness, claudication, myelopathy or bladder/bowel incontinence. Symptoms may be exacerbated with postural changes and Valsalva maneuver. Many are asymptomatic incidental findings on imaging studies done for other reasons. The etiology of these cysts is debated.
Epidural cysts are most commonly located posteriorly and displace the dura. Larger lesions may cause symptoms by compressing the spinal cord. Most occur in the thoracic spine posteriorly. There may be erosion of the adjacent bony elements of the spinal canal. Synovial cysts are not arachnoid cysts but appear as epidural cysts that can be characterized because of their proximity to diseased facet joints and thick walls.
Extramedullary intradural cysts are even less common than epidural cysts and are mostly located posteriorly in the spine. They can be classified as primary or associated with trauma, infection or subarachnoid hemorrhage. Extramedually intradural cysts are difficult to visualize on MRI and CT because of their similarity in signal intensity or density of the cyst fluid to CSF. Since these cysts to do not enhance, intravenous contrast is not helpful. Discovery of these lesions primarily relies on identification of displacement of adjacent structures. Extramedullary cysts located anteriorly are even less common. Cine-MRI has been reported to be helpful for diagnosis. In this case however, CSF flow study did not reveal differential flow between the cyst and the subarachnoid spaces above or below the cyst. The cyst could not be distinguished from CSF on a multi-echo sequence (TR 2000 TE 16,32,48,64, not shown.) Most subarachnoid cysts communicate with the subarachnoid space. In this case, communication was not demonstrated on the delayed CT-myelogram (shown above) which did not reveal contrast penetration into the cyst. Rarely, a hydatid cyst could mimic an arachnoid cyst, and may be suspected when the cyst wall is markedly hypointense on T1 and T2 weighted images.
Intramedullary cysts can be easily differentiated from intradural cysts. CT may demonstrate a low density cystic cavity, with or without cord enlargement. Intramedullary cysts are easily visualized on MRI because of the differential signal intensity between cyst and surrounding spinal cord. Intravenous gadolidium based contrast agent may be helpful in cases related to neoplasia. Intramedullary cysts may be congenital, benign, post traumatic, or neoplastic. Spinal intradural cysts related to trauma or surgery can be associated with an intramedullary cyst.
Conservative management is recommended for cysts found incidentally. Symptomatic intradural cysts are treated with surgical excision. An important component of surgical treatment of epidural cysts includes closure of the arachnoid defect that is the source of the CSF leak.